Hospitals and insurance giants are clashing over wildly popular Medicare Advantage plans as both sides try to protect their profits. Many seniors enrolled in these plans are caught in the crosshairs.
More hospitals and healthcare providers are terminating agreements with insurers that provide these private-sector alternatives to Medicare, citing too many denials, delays, and refusals to pay for care that government-run health insurance would typically cover.
The fracas is deepening this year as the federal government issues new guidance on how the plans can be run, posing a major new threat to a profit engine for some of the country’s largest insurance companies.
“We call these knife fights in the industry and I think we’re seeing more and more,” Whit Mayo, an analyst with Leerink Partners, told Yahoo Finance. “And is this something that these insurers are going, ‘OK, this could become a bigger problem for our bottom line.'”
Seniors also have a lot at stake. If more hospitals ditch these plans, seniors who rely on that coverage will be forced to pay higher costs or may even be kept from seeing the doctor of their choice. Many have little recourse if they face these challenges.
“It stinks,” Mayo said. “You’re putting consumers in the middle of these negotiations and they really value being able to know if they’re facing out-of-network costs if they do see a provider that’s not within their network. So the emotional strain that this takes on the people caught in the middle is the worst.”
‘The deck is heavily stacked in favor of MA enrollment’
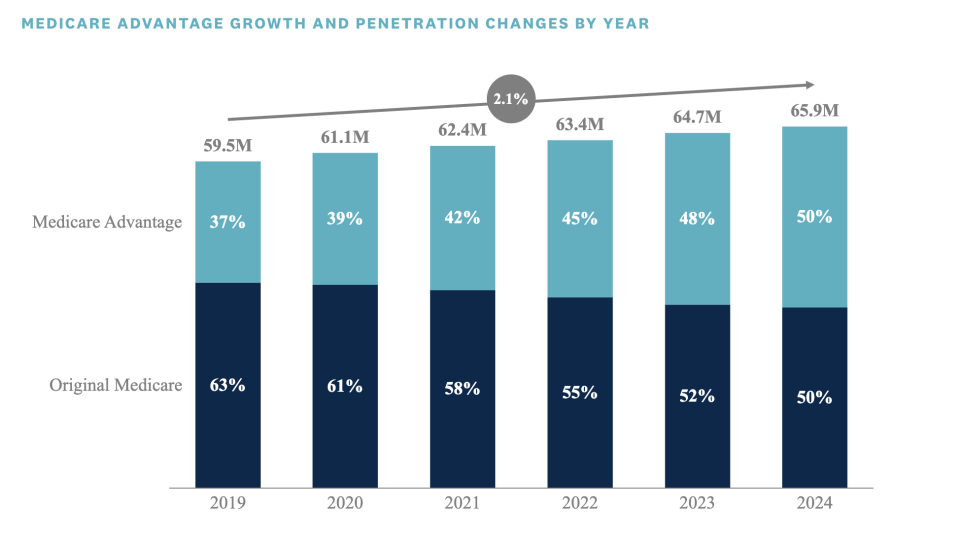
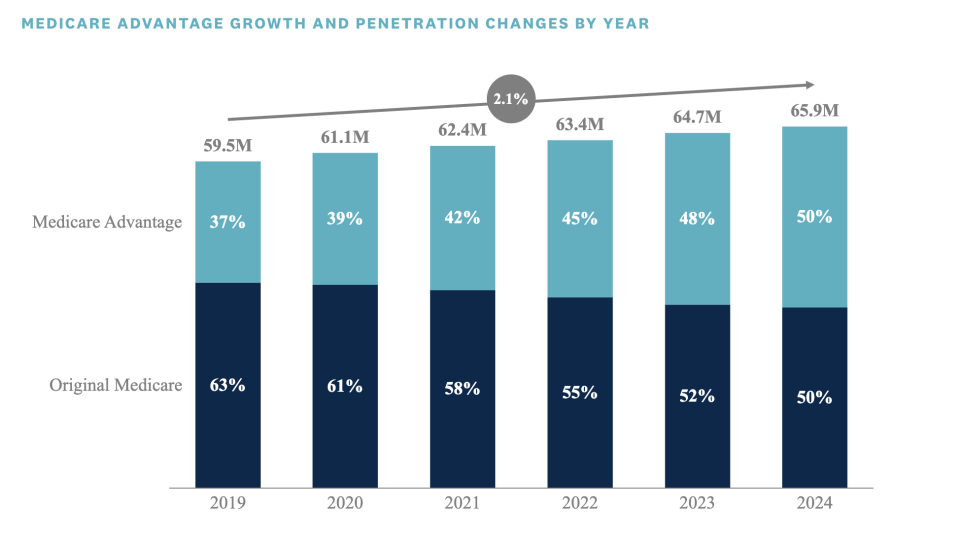
This year, 33 million Americans have MA plans, representing just over half of Medicare-eligible individuals, according to research from Chartis. They are offered by giant companies like UnitedHealthcare, which is owned by UnitedHealth Group (UNH), as well as Humana (HUM) and CVS/Aetna (CVS).
These MA plans have only grown in popularity since the program’s inception, with enrollment outpacing that of traditional Medicare in the last six years. Two big allures of these plans are their perks and cost.
MA plans provide benefits traditional Medicare doesn’t offer, such as dental and vision coverage and a grocery allowance. Many also offer a low or $0 monthly premium. That’s cheaper than Medicare’s $174.70 monthly premium and any supplemental coverage seniors who choose Medicare often buy.
“MA plans are very well compensated. With that extra money, MA plans are able to offer services that Medicare doesn’t offer,” David Lipschutz, the associate director for the Center for Medicare Advocacy, told Yahoo Finance. “The deck is heavily stacked in favor of MA enrollment.”
Of course, there’s a tradeoff. Depending on the MA plan, enrollees have to go to a network of providers who have contract agreements with the insurer. If an enrollee goes out of network, they either must pay higher costs for the care or may not be allowed to see that provider at all.
‘They deny it’
The consequences of that tradeoff came to a head in 2022 as MA insurers began denying more coverage for necessary care just as seniors who had delayed elective procedures flooded back into hospitals that were already struggling with major labor shortages.
The practice has infuriated healthcare providers.
“This practice does cost substantial amounts of time and money, but more important, it’s not right for our patients who are often caught in the middle or receive coverage that is different than that offered to patients enrolled in traditional Medicare,” wrote a spokesperson for Louisville, Ky.-based Baptist Health Medical Group, which last year terminated its MA agreement with Humana.
Some hospitals move forward with care without prior authorization because it’s an emergency and the appeals process takes too much time.
“There are patients out there that can’t wait. The delay of a cardiac procedure or cancer procedure could be life-threatening,” said Chris Van Gorder, the president and CEO of San Diego-based Scripps Health.
And when the hospital files a claim, “They deny it saying, ‘We didn’t approve it,'” Van Gorder said.


‘Going to get ugly’
Many healthcare providers are losing money as a result.
Scripps Health lost $75 million last year from its MA-insured patients, Van Gorder said.
Scripps Clinic and Scripps Coastal, the medical groups that have exclusive medical service contracts with Scripps Health, tried to renegotiate with MA insurers to reach acceptable terms, but that ultimately wasn’t successful.
The medical groups then withdrew from their MA HMO agreements with UnitedHealthcare, Anthem Blue Cross, Blue Shield of California, Health Net of California, SCAN Health Plan, UnitedHealthcare of California, and Alignment Health last year.
“The last thing in the world I wanted to do is cancel a contract for 32,000 patients. I’m in the business of delivering healthcare, not canceling healthcare,” Van Gorder said. “We just can’t afford it financially.”
In the last 18 months, more than a dozen other healthcare and hospital systems nationwide have dropped out of MA plan networks, many of them citing denial-of-care issues.
“I think we are sadly the vanguard of what is going to be some pretty confrontational contract negotiations between payers and hospitals in the next few years,” Van Gorder said. “I think this is going to get ugly.”


UnitedHealthcare told Yahoo Finance that “each year, we successfully renegotiate the vast majority of our contracts with providers. Our goal is to be a good steward of the resources available to cover our members’ cost of care by ensuring they are charged fair, sustainable prices for the services they need.”
Humana and Centene did not respond to requests for comment.
Still, the tumult also has gotten the attention of the Centers for Medicare & Medicaid Services, which recently put out new rules on processing prior authorizations, patient risk coding, and other reporting and transparency requirements designed to address some of the medical providers’ concerns.
It also adds more pressure on insurers by making it harder to deny claims, potentially forcing insurers to cut back on the perks their MA plans offer.
“The industry is engulfed in just a historically high level of controversies right now. It’s a very tough environment for the plans,” Mayo said. “And I think we’re going to see a sector that’s going to really pull back on benefits.”
‘People don’t have much recourse’
In the meantime, seniors who need healthcare are stuck in the middle.
Seniors can opt for a different MA plan or original Medicare during the Medicare Advantage open enrollment period from Jan. 1 to March 31 — and they have been. Plan swapping was up in January and February, Mayo said, based on monthly data from the CMS.
Still, switching to traditional Medicare is no panacea, either. While seniors will have no problem getting Medicare, they may find it harder to get a Medigap policy, a supplemental policy that covers the 20% of costs that Medicare does not cover for medical care.
When a senior first signs up for Medicare at age 65, Medigap policies — which are provided by many of the insurers that offer MA plans — cannot deny or charge a higher premium based on preexisting conditions.
But insurers can deny or charge more for preexisting conditions when someone wants to switch to traditional Medicare down the road. That’s why seniors may choose another MA plan instead, one that could be dumped later by their medical provider.
“That is a danger each and every year,” Lipschutz said. “People don’t have much recourse if their doctor leaves the network.”
Janna Herron is a Senior Columnist at Yahoo Finance. Follow her on Twitter @JannaHerron.
Click here for in-depth analysis of the latest stock market news and events moving stock prices.
Read the latest financial and business news from Yahoo Finance
















